8/7/18
Invasive new tick is spreading in the US
An invasive new tick is spreading in the US
https://www.wral.com/an-invasive-new-tick-is-spreading-in-the-u-s-/17750702
By Donald G. McNeil Jr., New York Times
The Asian long-horned tick, Haemaphysalis longicornis, is spreading rapidly along the Eastern Seaboard. It has been found in 7 states & in the heavily populated suburbs of New York City.
At the moment, public health experts say they're concerned, but not alarmed.
Although domestic U.S. ticks are a growing menace & transmit a dozen pathogens, no long-horned ticks here have yet been found with any human diseases. In Asia, however, the species carries a virus that kills 15% of its victims.
Known in Australia as bush ticks & in New Zealand as cattle ticks, long-horned ticks can multiply rapidly & suck so much blood from a young animal that it dies. The ticks bloat up like fat raisins until their tiny legs are barely able to support them.
After a blood meal, females can lay hundreds of fertile eggs without mating.
“One tick can crank out females in fairly large numbers,” said Thomas Yuill, a retired pathobiologist at the University of Wisconsin, Madison, who was one of the first to raise alarms about the invaders.
The first long-horned tick was found last summer in western New Jersey. This summer they were collected in public parks & a golf course in Bergen, Essex and Middlesex counties in New Jersey, & in wooded & grassy areas of New York’s Westchester County.
They were reported in Pennsylvania for the first time last week, & have been sighted in Arkansas, North Carolina, Virginia & West Virginia.
They were found feeding on horses, dogs, deer, a calf, a sheep & an opossum. They do bite humans, but it isn't clear how often.
People should use the same precautions they do against domestic ticks, experts said, such as using repellents & checking for ticks after walking through woods or tall grass.
Tadhgh Rainey, an entomologist at the public health department of Hunterdon County, New Jersey, found the first long-horned ticks in the country last August, when a woman who'd been shearing her pet Icelandic sheep came to his department with ticks on her hands and wrists.
“I thought she’d have a few,” Rainey said in an interview. “But she was covered in them, easily over 1,000 on her pants alone.”
Most were young nymphs about the size of dust specks. “She had a change of clothes in her car, so we put her clothes in the freezer to kill them,” Rainey recalled.
The ticks didn’t match any North American pests, & initially he couldn't identify them. The woman’s 12-year-old sheep was penned alone & had never traveled, so where they came from remained a mystery.
A month later the woman called again to see if he'd figured out what they were, & Rainey drove out to see the animal for himself. “A minute after we entered the paddock, even before I touched the sheep, I was covered in ticks,” he said.
The sheep was weak from blood loss, so he gave the owner some insecticidal livestock wash. The grass around the paddock was later cut & the area sprayed in an effort to eliminate the outbreak.
Andrea Egizi, an entomologist at Rutgers University, finally identified the longhorns by DNA analysis. Her lab has now tested more than 100 specimens found in New York & New Jersey.
Thus far, Egizi said, none have any of the pathogens causing the 6 diseases she screens for: Lyme disease, relapsing fever, babesiosis, anaplasmosis & 2 varieties of erlichiosis.
The Centers for Disease Control & Prevention lab in Fort Collins, Colorado, has screened about 100 long-horned ticks for 3 dangerous viruses — Powassan, Heartland & Bourbon — & all came up negative, said Ben Beard, the agency’s deputy director of vector-borne diseases.
The lab now has 10 live longhorns & is feeding them to create a colony, Beard said. That will take about a year, & then researchers can determine whether they can transmit Rocky Mountain spotted fever & other diseases.
In East Asia, long-horned ticks do carry pathogens related to Lyme & others found in North America. But the biggest threat is a phlebovirus that causes SFTS, for severe fever with thrombocytopenia syndrome. (Thrombocytopenia means abnormally low levels of platelets, which help the blood clot; a severe drop triggers internal bleeding and organ failure.)
The syndrome has an overall fatality rate of about 15%, said Terry A. Klein, an entomologist working with the U.S. military in South Korea. But SFTS is more lethal to people aged 60 or older, killing half of them.
However, the syndrome isn't found in Australia or New Zealand, earlier stops for the long-horned ticks as they spread from Asia. In those countries, they cause babesiosis & theileriosis in cattle but are mostly “of nuisance value” to humans, said Dr. David Thomson, a veterinarian in Queensland, Australia.
It’s not clear that the SFTS virus, which is related to the Heartland virus found in a number of U.S. states, could get established in this country, because its transmission cycle is unknown — it may need more than one host.
It’s not known when or how long-horned ticks reached the United States, nor why the species is spreading so fast now. They bite birds, but Rainey said he suspected they originally arrived on a large animal. As far back as 1960, he said, the ticks were found on a horse held in quarantine.
One collected in 2013, Beard said, was misidentified until recently as a rabbit tick, which is also in the Haemaphysalis genus.
In theory, just one female could have produced all the long-horned ticks spreading in the country through asexual reproduction. But Egizi said she has found 3 mitochondrial DNA lineages, meaning at least 3 females arrived.
Although experts said having a new invader is unsettling, they worry more about deer ticks, lone star ticks & other established species whose ranges are growing as winters get warmer.
Cases of the illnesses they transmit — everything from Lyme disease to alpha-gal, an allergy to red meat — are increasing rapidly. Even in Asia, only about 1% of long-horned ticks have the SFTS virus; in parts of this country, 25% of deer ticks carry Lyme disease.
“The jury’s still out on how big a threat this is,” Beard said. “But we think it’s a very important question to address.”
5/6/17
Powassan Virus Contracted Through Tick Bites on Rise
Experts warn of increases in tick-borne Powassan virus
http://www.cnn.com/2017/05/03/- Anyone bitten by an infected tick is susceptible to the rare virus
- The virus can be fatal in up to 15% of cases with symptoms, one doctor warns
(CNN) Summer
is nearly here, & it's bringing fears of a rare tick-borne disease
called Powassan. This potentially life-threatening virus is carried &
transmitted by 3 types of ticks, including deer tick that
transmits Lyme disease.
Over
past decade, 75 cases were reported in northeastern states &
Great Lakes region.
Warmer winters result in increases in the tick
population, so experts predict rising tick-borne infections of many
types.
Everyone
is at risk for Powassan. Infections are most likely during late spring, early summer
&
mid-fall, when ticks are most active.
About
15% of patients who are infected & have symptoms are not going
survive. Of survivors, at least 50% will have
long-term neurological damage that is not going to resolve."
Although
most infected people will never show symptoms, those who do become sick
usually do so a few days to about a week after tick bite.
The most common symptoms will be fever & headache.
The
unlucky few who develop a more serious illness will do so very quickly
over next couple of days. You start to develop
difficulties with maintaining your consciousness & your cognition. ...
You may develop seizures. You may develop inability to breathe on your
own.
Just as there are no vaccines to prevent infection, there are also no treatments for Powassan.
Standard treatment includes intravenous fluids, though antiviral medications, systemic corticosteroids & other drugs have been tried in some patients. Scientists
also believe Powassan is on rise based on studies that have
identified an increasing number of infections in deer.
There are more & more deer that they're finding
that have been infected with this virus.
Similarly, Lyme is showing increasing numbers.
Prevention is first step
The Powassan virus was first discovered in Ontario in 1958. A child came down with an unspecified encephalitis," or brain inflammation. When the never-seen-before virus was identified,
scientists called it Powassan after town where child lived.
Dr.
Daniel Pastula, an assistant professor of neurology, medicine
(infectious diseases) & epidemiology at University of Colorado
Denver & Colorado School of Public Health, explains that of 3 ticks
that can carry Powassan -- Ixodes cookei, Ixodes marxi & Ixodes
scapularis -- the third "likes to bite humans" the most.
Commonly known as a deer tick, Ixodes scapularis can also bite mice, Pastula explained.
"The
thought is maybe that is where it gets Powassan from," he said. The
virus may enter cycle between ticks & small & medium-size forest
rodents that live up in Great Lakes & Northeast, & "humans just
happen to be occasionally involved in that cycle."
"Unless you're an entomologist, it's very hard to identify ticks. They're kind of small," he said.
"The
best thing people can do if they're worried about Powassan or any other
tick-borne virus is to prevent against all tick bites," Pastula said.
This
is best done by avoiding high brushy areas whenever you're in the
woods, wearing long sleeves & pants when feasible, using insect
repellent & doing tick checks after being outdoors, he said.
"It
has to be insect repellent that is actually shown to work. Repellents containing
DEET or picaridin or IR3535 are recommended ones, according to EPA & CDC," Pastula said.
"Essentially, you don't need to worry about Powassan if you don't get bit by a tick," he said.
3/5/17
Rocky Mountain Spotted Fever (RMSF) - Grave Illness Caused by Ticks

Rocky Mountain spotted fever (RMSF) is a disease caused by infection with bacterium Rickettsia rickettsia which is transmitted by a bite from infected ticks.
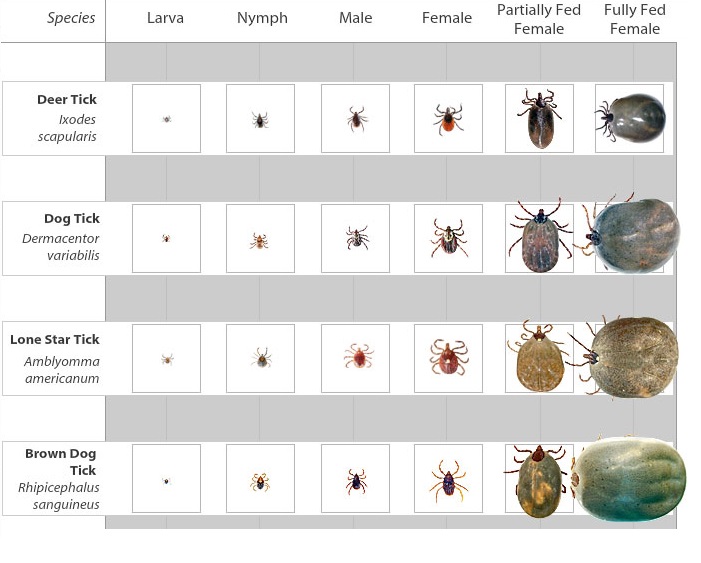
Three (3) species of ticks have been identified to be carriers of this bacterium:
Rocky mountain wood tick (Dermacentor andersoni), American dog tick (Dermacentor variabilis), and the Brown dog tick (Rhipicephalus sanguineus).

These are a female (left) and male (right) Rocky Mountain Wood Tick (Dermacentor andersoni).

Female (left) and male (right) American dog tick (Dermacentor variabilis)

Brown dog tick (Rhipicephalus sanguineus) (female on left, male on right).
Below is a link to a website dedicated to Rocky Mountain Fever:
http://www.aldf.com/rocky-mountain-spotted-fever
Below is some information from that website regarding this illness.
What is Rocky Mountain Spotted Fever?
Rocky Mountain spotted fever (RMSF) is most serious tick-borne disease in US & is caused by Rickettsia rickettsii, a type of bacteria known as rickettsia. These bacteria are transmitted to humans by bite of certain hard ticks.The 2 most important species of ticks that can transmit R. rickettsii in United States are Dermacentor variabilis (American dog tick) & Dermacentor andersoni (Rocky Mountain wood tick).
A third species, Rhipicephalus sanguineus (brown dog tick) has been implicated as a vector.

Dogs are susceptible to RMSF, & sometimes household members of infected dogs may also be at risk for acquiring disease. In countries south of US, cayenne tick (Amblyomma cajennense) has also been shown to act as a vector of RMSF.
More recently another rickettsie has been identified as cause of a spotted fever-like disease. Theis species, called Rickettsia parkeri, was first identified more than 60 years ago in Amblyomma maculatum ticks (Gulf coast ticks).
Confirmation of R. parkeri as a causative agent of human disease occurred in 2002 when serological (blood) tests, immunohistochemical staining, cell culture isolation & other molecular tests positively verified infection in a patient.
The classic symptoms of RMSF include fever & a spotted (petechial) rash, although they aren't always present. RMSF can be a fatal disease & patients often require hospitalization.
Severe illness is seen more often in patients who delay seeking care from a physician because such patients don't receive antibiotic treatment as soon as they should.
RMSF is considered an acute infection & infection with Rickettsia rickettsii is thought to provide long-lasting immunity against re-infection, however this shouldn't deter those who feel they suffer symptoms from seeking care.
RMSF is typically treated with a course of tetracycline antibiotics (CDC).
Where is Rocky Mountain Spotted Fever Prevalent?
Although first recognized in late 19th century in Rocky Mountain region, by 1930s this disease was found to be present in eastern portion of country as well.The wood tick (Dermacentor andersoni), one of main tick vectors is found in Rocky Mountain states& southwestern Canada. The second major vector is American dog tick (Dermacentor variabilis).

This tick is distributed east of Rocky Mountains & in some regions along Pacific Coast.
The cayenne tick (Amblyomma cajennense) is found in South & Central America; however its range also extends into some southern states including Texas.
The most recently implicated vector of R. parkeri is lone star tick (Amblyomma americanum). It is found in southern states as well as along East coast up to Maine.
There has been a marked drop in incidence of RMSF in Rocky Mountain States since 1940s. Today over half of cases of RMSF occur in South Atlantic states (Delaware through Florida).
Rocky Mountain spotted fever is a seasonal disease with majority of cases occurring between months of April & September. Clustered cases of RMSF have occurred among families in states including Kentucky, Arizona & Oklahoma.

Rocky Mountain spotted fever is a nationally notifiable disease to CDC, & cases are reported via 2 national surveillance systems, standardized case report forms & National Electronic Telecommunications System for Surveillance (NETSS).
Cases are considered confirmed or probable based on results of lab tests. Over last 50 years approximately 250 to 1200 cases have been reported annually.
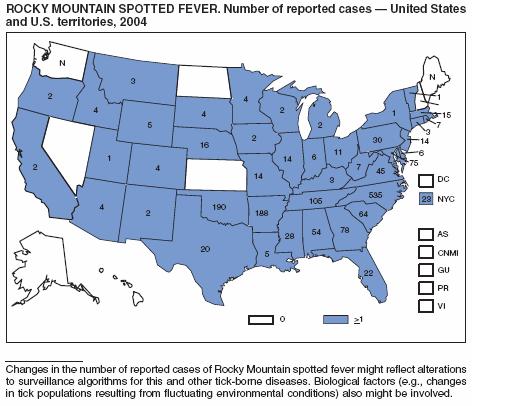
Image obtained from CDC MMWR Report
Symptoms
Symptoms of Rocky Mountain spotted fever usually appear 2 to 14 days (average of 7 days) after being bitten by infected tick.Fever is often first symptom experienced by patients. The classic triad of fever, rash & tick bite is present among many but not all cases at initial visit to physician.
Nausea, vomiting, severe headache, muscle pain & lack of appetite are also sometimes reported by patients in early stage of disease.
Other clinical symptoms include abnormal platelet count (thrombocytopenia), elevated liver enzymes, & electrolyte abnormalities.
The initial rash tends to appear 2 or 3 days after onset of illness as small pink non-itchy spots (macules) on skin that later become characteristic spotted red rash (petechiae).

The rash is most often found on ankles& wrists & then appears on trunk, palms & soles. The characteristic petechial rash occurs in only 35 to 60% of patients, & as many as 10 to 15% of patients may never develop a rash. Other late stage symptoms associated with RMSF include abdominal pain, joint pain, & diarrhea.
Long term consequences of RMSF include paralysis of lower extremities, hearing loss, loss of bowel or bladder control, loss of limbs through amputation, movement disorders, & language disorders.
If left untreated RMSF can be fatal.
Symptoms of spotted fever like disease caused by most recently implicated rickettsia, R. parkeri, are very similar to those caused by R. rickettsii.
However, while lesions (called eschars) at site of tick bite rarely occur in R. rickettsii-associated RMSF, they do occur in infections caused by R. parkeri.
Diagnosis
Clinical diagnosis of RMSF is based on serological tests including detection of antibody titers via IFA, detection of bacterial agent via culture or immunohistochemical staining of biopsies, & by detection of bacterial DNA in a clinical specimen via PCR.However, treatment decisions shouldn't be delayed while waiting for confirmation with lab results. Patients with a relevant history & symptomology should be treated with appropriate antibiotic regimen immediately.
Since R. rickettsii & R. parkeri bacterial species are so closely related, cross-reactivity between these 2 agents may make it difficult to distinguish between them using less specific serological or immunohistochemical assays.
Treatment
Upon suspicion of Rocky Mountain spotted fever, treatment should begin immediately. Delay of treatment has been associated with fatal outcomes.Treatment with tetracycline or chloramphenicol antibiotics can be used to treat RMSF. Doxycycline (a tetrycycline) antibiotic is treatment of choice for both adults & children. However doxycycline isn't recommended for use by pregnant women.
Current recommendations from Centers for Disease Control & Prevention (CDC) include doxycycline therapy for 5 to 10 days. Complicated disease cases may require longer treatment. Patients usually see an improvement in fever 24 to 72 hours after starting antibiotics.


8/31/16
Update: June 2016 - Tickborne Diseases of United States
Tickborne Diseases of United States
http://www.cdc.gov/ticks/diseases/index.html
- Anaplasmosis is transmitted to humans by tick bites primarily from blacklegged tick (Ixodes scapularis) in northeastern & upper midwestern U.S. & western blacklegged tick (Ixodes pacificus) along Pacific coast.
http://www.cdc.gov/anaplasmosis- Anaplasmosis is a tickborne disease caused by bacterium Anaplasma phagocytophilum. It was previously known as human granulocytic ehrlichiosis (HGE) & has more recently been called human granulocytic anaplasmosis (HGA). Anaplasmosis is transmitted to humans by tick bites primarily from black-legged tick (Ixodes scapularis) & western black-legged tick (Ixodes pacificus). Of 4 distinct phases in tick life-cycle (egg, larvae, nymph, adult), nymphal & adult ticks are most frequently associated with transmission of anaplasmosis to humans. Typical symptoms include: fever, headache, chills, & muscle aches. Usually, these symptoms occur within 1-2 weeks of a tick bite. Anaplasmosis is initially diagnosed based on symptoms & clinical presentation, & later confirmed by use of specialized lab tests. The first line treatment for adults & children of all ages is doxycycline. Anaplasmosis & other tickborne diseases can be prevented.
- Babesiosis is caused by microscopic parasites that infect red blood cells. Most human cases of babesiosis in U.S. are caused by Babesia microti. Babesia microti is transmitted by blacklegged tick (Ixodes scapularis) & is found primarily in northeast & upper midwest.
- http://www.cdc.gov/parasites/babesiosisBabesiosis is caused by microscopic parasites that infect red blood
cells & are spread by certain ticks. In United States, tickborne
transmission is most common in particular regions & seasons: it mainly
occurs in parts of Northeast & upper Midwest & usually peaks
during warm months.
Although many people who are infected with Babesia don't have symptoms, for those who do effective treatment is available. Babesiosis is preventable, if simple steps are taken to reduce exposure to ticks.
Babesia microti is transmitted by bite of infected Ixodes scapularis ticks—typically, by nymph stage of tick, which is about size of a poppy seed. - Borrelia mayonii infection has recently been described as a cause of illness in upper midwestern United States. It has been found in blacklegged ticks (Ixodes scapularis) in Minnesota & Wisconsin. Borrelia mayonii is a new species & is only species besides B. burgdorferi known to cause Lyme disease in North America.
http://www.cdc.gov/ticks/mayonii.html
What you need to know about Borrelia mayonii
In 2013, scientists at Mayo Clinic noticed an unusual result while testing blood from patients suspected of having Lyme disease. Cooperation between Mayo Clinic, state public health agencies, & CDC confirmed discovery as a new bacterial species, also found in blacklegged ticks. Joint efforts between these groups are currently underway to find more patients infected with this bacteria, to look for additional areas where infected ticks live, & to identify other bacteria that cause tickborne disease.
What is Borrelia mayonii?
Borrelia mayonii is proposed name for a new bacteria species recently found to cause Lyme disease in 6 people who live in upper Midwestern United States. Worldwide, Lyme disease is caused by 3 main species of bacteria: Borrelia burgdorferi, B. afzelii, and B. garinii. Borrelia burgdorferi causes Lyme disease in United States, while other 2 species are leading causes of Lyme disease in Europe & Asia. Borrelia mayonii is a new species that is genetically distinct from these 3 species & is only species besides B. burgdorferi shown to cause Lyme disease in North America. Regardless of bacteria’s species, illness is still called Lyme disease or Lyme borreliosis.
How was it discovered?
The new bacteria species was first identified at Mayo Clinic in Rochester, Minnesota, where diagnostic samples from patients were tested for evidence of Lyme disease using a well-described polymerase chain reaction (PCR) assay. From 2012 through 2014, six of approximately 9,000 diagnostic samples from residents of Minnesota, Wisconsin, & North Dakota revealed presence of a genetically distinct bacteria. Scientists analyzed DNA sequences of these bacteria & found that they belonged to a new species of Borrelia. Blood from 2 of patients was also tested by culture at CDC, & organism was successfully grown in lab.
Where does B. mayonii occur?
Current evidence suggests that B. mayonii is only found in upper Midwestern United States. The new species wasn't identified in any of approximately 25,000 samples submitted from patients living in 43 other states, including states in Northeast & Mid-Atlantic region where Lyme disease is common.
Has B. mayonii been found in ticks?
Yes. B. mayonii has been identified in blacklegged (or “deer”) ticks collected in several counties in northwestern Wisconsin & Minnesota. It is highly likely, however, that infected ticks occur in other areas of both states. The black-legged tick (Ixodes scapularis) also transmits B. burgdorferi, agents that cause anaplasmosis & babesiosis, & Powassan virus.
What type of illness does B. mayonii cause?
Limited information from first 6 patients suggests that illness caused by B. mayonii is similar to that caused by B. burgdorferi, but with a few possible differences. Like B. burgdorferi, B. mayonii causes fever, headache, rash, & neck pain in early stages of infection (days after exposure) & arthritis in later stages of infection (weeks after exposure). Unlike B. burgdorferi however, B. mayonii appears to be associated with nausea & vomiting, diffuse rashes, & a higher concentration of bacteria in blood.
What tests are used to diagnose B. mayonii?
Lyme disease, including infection with B. mayonii, can be treated based on signs & symptoms & a history of possible exposure to ticks. Currently available information suggests that patients with B. mayonii infection develop a serologic response similar to that of patients infected with B. burgdorferi. Therefore, Lyme disease two-tier testing can be helpful for detecting infection with B. mayonii if used correctly & performed with FDA cleared tests. In some instances, B. mayonii spirochetes may also be seen on a blood smear. At this time, infection with B. mayonii can be specifically identified by Lyme disease PCR tests at Mayo Clinic.
How is B. mayonii treated?
Physicians have successfully treated patients infected with B. mayonii with a 2-4 week course of doxycycline. Amoxicillin, ceftriaxone, & cefuroxime have also been used.
Why are we just discovering this now?
Good question! The diagnostic lab at Mayo Clinic has tested approximately 100,000 patient samples in same way for over a decade but only recently detected evidence of B. mayonii. It is possible that bacteria recently emerged or that bacteria has been present in area for a long time but at levels so low it escaped detection.
I live in northeastern United States where Lyme disease is common. Should I be worried about B. mayonii?
At this time there is no evidence that B. mayonii is present outside of Upper Midwest. However, you should continue to take precautions against tick bites as Lyme disease, anaplasmosis, & babesiosis are well established in much of Northeast.
What more do researchers need to know?
CDC has initiated a project to detect & characterize species of bacteria in specimens from patients suspected of tickborne illness like Lyme disease. Over next several years, scientists aim to test 30,000 patient samples to gain more information about extent & clinical course of this illness.
In addition, entomologists will continue to sample ticks in Upper Midwest to determine geographic extent of ticks that are infected with this bacteria. CDC & state of Minnesota recently completed a field collection of ticks from 80 sites throughout Minnesota. Ticks will be screened for B. mayonii to determine how geographically widespread & how prevalent pathogen is in that state. Researchers also plan to test for B. mayonii in ticks that have been collected from other parts of country.
How can I avoid this disease?
People living in areas where blacklegged ticks are common should continue to take precautions against tick bites & see their physician if they experience fever, rash, or malaise after a tick bite or after spending time in tick habitat. Click here for more information.
- Borrelia miyamotoi infection has recently been described as a cause of illness in U.S. It is transmitted by blacklegged tick (Ixodes scapularis) & has a range similar to that of Lyme disease.
- Colorado tick fever is caused by a virus transmitted by Rocky Mountain wood tick (Dermacentor andersoni). It occurs in Rocky Mountain states at elevations of 4,000 to 10,500 feet.
http://www.cdc.gov/ticks/miyamotoi.html
What you need to know about Borrelia miyamotoi
What is Borrelia miyamotoi?
Borrelia miyamotoi is a species of spiral-shaped bacteria that is closely related to bacteria that cause tick-borne relapsing fever (TBRF). It is more distantly related to bacteria that cause Lyme disease. First identified in 1995 in ticks from Japan, B. miyamotoi has since been detected in 2 species of North American ticks, black-legged or “deer” tick (Ixodes scapularis) & western black-legged tick (Ixodes pacificus). These ticks are already known to transmit several diseases, including Lyme disease, anaplasmosis, & babesiosis.
What type of illness does B. miyamotoi cause?
In recently published research, patients with this infection were most likely to have fever, chills, & headache. Other common symptoms included body & joint pain & fatigue. Unlike Lyme disease, rash was uncommon, presenting in only 4 out of 51 patients.
What type of testing is available for patients who might be infected?
Blood tests for Lyme disease aren't helpful in diagnosis of B. miyamotoi infections. Currently, confirmation of a diagnosis relies on 1) use of polymerase chain reaction (PCR) tests that detect DNA from organism or 2) antibody-based tests. Both types of tests are under development & not widely commercially available but can be ordered from a limited number of CLIA-approved labs.
How is B. miyamotoi treated?
Physicians have successfully treated patients infected with B. miyamotoi with a 2-4 week course of doxycycline. Amoxicillin & ceftriaxone have also been used.
What more do researchers need to know?
Researchers & health care providers need more information about signs & symptoms of this infection. Fewer than 60 well-documented cases of human infection have been reported in United States to date.
It is also unclear how common this infection is in United States. Improved means of diagnosing B. miyamotoi disease will help researchers learn how many people are affected by it.
What is CDC doing?
CDC is working to better define public health importance of this infection & is reviewing options for tracking disease with our partners in state & local health departments. CDC is also developing & evaluating lab diagnostic tests to detect presence of B. miyamotoi in infected individuals & measure their specific immune responses.
How can I avoid this disease?
The route of transmission of B. miyamotoi to humans hasn't been firmly established, but likely involves bite of infected black-legged ticks. People living in areas where blacklegged ticks are common should continue to take precautions against tick bites & see their physician if they experience fever, rash, or malaise after a tick bite or after spending time in tick habitat. For more information, visit CDC’s Ticks site.
- http://www.cdc.gov/coloradotickfever
- Ehrlichiosis is transmitted to humans by lone star tick (Ambylomma americanum), found primarily in southcentral & eastern U.S.Colorado tick fever (CTF) virus is spread to people through bites of infected ticks. People who live in or visit areas in western United States or western Canada that are 4,000‒10,000 feet above sea level may be at risk of becoming infected. Most cases of CTF occur during spring & summer months when ticks are most active. The most common symptoms of CTF are fever, chills, headache, body aches, & feeling tired. There are no medications to treat or vaccines to prevent CTF.
The best way to prevent CTF is to reduce your risk of tick bites.
- Use insect repellent
- Wear long sleeves & pants
- Avoid wooded & bushy areas with high grass
- Perform thorough tick checks after spending time outdoors
- http://www.cdc.gov/ehrlichiosis
- Ehrlichiosis is general name used to describe several bacterial diseases that affect animals & humans. Human ehrlichiosisis a disease caused by at least 3 different ehrlichial species in United States: Ehrlichia chaffeensis, Ehrlichia ewingii, & a third Ehrlichia species provisionally called Ehrlichia muris-like (EML). Ehrlichiae are transmitted to humans by bite of an infected tick. The lone star tick (Amblyomma americanum) is primary vector of both Ehrlichia chaffeensis & Ehrlichia ewingii in United States. Typical symptoms include: fever, headache, fatigue, & muscle aches. Usually, these symptoms occur within 1-2 weeks following a tick bite. Ehrlichios is diagnosed based on symptoms, clinical presentation, & later confirmed with specialized lab tests. The first line treatment for adults & children of all ages is doxycycline. Ehrlichiosis & other tickborne diseases can be prevented.
- Heartland virus infection has been identified in 8 patients in Missouri & Tennessee as of March 2014. Studies suggest that Lone Star ticks may transmit virus. It is unknown if virus may be found in other areas of U.S.
- http://www.cdc.gov/ncezid/dvbd/heartland/index.html
What is Heartland virus?
Heartland virus belongs to a family of viruses called Phleboviruses. Viruses in this family are found all over world. Some of these viruses can cause people to get sick. Most of phleboviruses that cause people to become ill are passed through bite of a mosquito, tick, or sandfly.
How do people get infected with Heartland virus?
It isn't yet fully known how people become infected with Heartland virus. However, recent studies suggest that ticks, namely Lone Star ticks, may transmit virus.
Where have cases of Heartland virus disease occurred?
As of March 2014, eight cases of Heartland virus disease have been identified among residents of Missouri & Tennessee. It is unknown at this time if virus may be found in other areas of United States.
What are symptoms caused by Heartland virus?
Since Heartland virus disease was first described in 2012 & there have only been a few cases, scientists are still learning about it. So far, all patients diagnosed with Heartland virus disease became sick during May-September. They all had a fever & felt very tired. Some also complained of headaches, muscle aches, diarrhea, losing their appetite, or feeling sick to their stomach. They all had low numbers of cells that fight infection & that help blood clot. Most patients required hospitalization for their illness. Most patients fully recovered, but one patient died.
Who is at risk for infection with Heartland virus?
People likely become infected with Heartland virus through a bite of a tick or other insect. Therefore, people who work or do activities outside, where they're exposed to ticks or insects, may be more likely to be infected.
How can people reduce chance of getting infected with Heartland virus?
There is no vaccine or drug to prevent or treat disease. Preventing bites from ticks & mosquitoes may prevent this & other infections.- Use insect repellents
- Wear long sleeves & pants
- Avoid bushy & wooded areas
- Perform thorough tick checks after spending time outdoors
- Lyme disease is transmitted by blacklegged tick (Ixodes scapularis) in northeastern U.S. & upper midwestern U.S. & western blacklegged tick (Ixodes pacificus) along Pacific coast.
- http://www.cdc.gov/lyme
- Lyme disease is caused by bacterium Borrelia burgdorferi & is transmitted to humans through bite of infected blacklegged ticks. Typical symptoms include fever, headache, fatigue, & a characteristic skin rash called erythema migrans. If left untreated, infection can spread to joints, heart, & nervous system. Lyme disease is diagnosed based on symptoms, physical findings (e.g., rash), & possibility of exposure to infected ticks. Lab testing is helpful if used correctly & performed with validated methods. Most cases of Lyme disease can be treated successfully with a few weeks of antibiotics. Steps to prevent Lyme disease include using insect repellent, removing ticks promptly, applying pesticides, & reducing tick habitat. The ticks that transmit Lyme disease can occasionally transmit other tickborne diseases as well.
- Powassan disease is transmitted by blacklegged tick (Ixodes scapularis) & groundhog tick (Ixodes cookei). Cases have been reported primarily from northeastern states & Great Lakes region.
- http://www.cdc.gov/powassan
- Powassan (POW) virus is transmitted to humans by infected ticks.
Approximately 60 cases of POW virus disease were reported in United
States over past 10 years. Most cases have occurred in Northeast & Great Lakes region. Signs & symptoms of infection can include
fever, headache, vomiting, weakness, confusion, seizures, & memory
loss. Long-term neurologic problems may occur. There is no specific
treatment, but people with severe POW virus illnesses often need to be
hospitalized to receive respiratory support, intravenous fluids, or
medications to reduce swelling in brain.You can reduce your
risk of being infected with POW virus by using tick repellents, wearing
long sleeves & pants, avoiding bushy & wooded areas, & doing
thorough tick checks after spending time outdoors. If you think you or a
family member may have POW virus disease, it is important to consult
your healthcare provider.
Rickettsia parkeri rickettsiosis is transmitted to humans by Gulf Coast tick (Amblyomma maculatum). - http://www.cdc.gov/otherspottedfever
- In addition to Rickettsia rickettsii, agent of Rocky Mountain spotted fever (RMSF), several other tick-borne species of Rickettsia, broadly grouped under heading "Spotted Fever group Rickettsia (SFGR)" have been shown to cause human infections. Tick-borne SFGR are transmitted to humans by bite of an infected tick, & may cause similar signs & symptoms to those observed for RMSF. These pathogens include several species of Rickettsia found in United States, including R. parkeri & Rickettsia species 364D (Table1). In addition, numerous tick-borne SFGR pathogenic to humans have been described internationally, including but not limited to R. conorii & R. africae (Table 2). Travelers may be at risk for exposure to these pathogens when engaging in behaviors that place them at risk for tick exposure, & physicians should maintain awareness of these diseases when a patient presents with a febrile illness within 2 weeks of returning home. Rickettsial infections with R. africae have been reported as a common cause of fever in travelers returning from South Africa.
- Rocky Mountain spotted fever (RMSF) is transmitted by American dog tick (Dermacentor variabilis), Rocky Mountain wood tick (Dermacentor andersoni), & brown dog tick (Rhipicephalus sangunineus) in U.S. The brown dog tick & other tick species are associated with RMSF in Central & South America.
- http://www.cdc.gov/rmsf
- Rocky Mountain spotted fever (RMSF) is a tickborne disease caused by bacterium Rickettsia rickettsii. This organism is a cause of potentially fatal human illness in North & South America, & is transmitted to humans by bite of infected tick species. In United States, these include American dog tick (Dermacentor variabilis), Rocky Mountain wood tick (Dermacentor andersoni), & brown dog tick (Rhipicephalus sanguineus). Typical symptoms include: fever, headache, abdominal pain, vomiting, & muscle pain. A rash may also develop, but is often absent in first few days, & in some patients, never develops. Rocky Mountain spotted fever can be a severe or even fatal illness if not treated in first few days of symptoms. Doxycycline is first line treatment for adults & children of all ages, & is most effective if started before 5th day of symptoms. The initial diagnosis is made based on clinical signs & symptoms, & medical history, & can later be confirmed by using specialized lab tests. RMSF & other tickborne diseases can be prevented.
- STARI (Southern tick-associated rash illness) is transmitted via bites from lone star tick (Ambylomma americanum), found in southeastern & eastern U.S.
- http://www.cdc.gov/stari
- A rash similar to rash of Lyme disease has been described in humans following bites of lone star tick, Amblyomma americanum. The rash may be accompanied by fatigue, fever, headache, muscle & joint pains. This condition has been named southern tick-associated rash illness (STARI). The cause of STARI isn't known.
- Tickborne relapsing fever (TBRF) is transmitted to humans through bite of infected soft ticks. TBRF has been reported in 15 states: Arizona, California, Colorado, Idaho, Kansas, Montana, Nevada, New Mexico, Ohio, Oklahoma, Oregon, Texas, Utah, Washington, & Wyoming & is associated with sleeping in rustic cabins & vacation homes.
- http://www.cdc.gov/relapsing-fever
- Relapsing fever is bacterial infection characterized by recurring
episodes of fever, headache, muscle & joint aches, & nausea. It is
caused by certain species of Borrelia spirochetes. There are 2 types of relapsing fever:
- Tick-borne relapsing fever (TBRF)
- Louse-borne relapsing fever (LBRF)
- Tularemia is transmitted to humans by dog tick (Dermacentor variabilis), wood tick (Dermacentor andersoni), & lone star tick (Amblyomma americanum). Tularemia occurs throughout U.S.
- http://www.cdc.gov/tularemia
- Tularemia is a disease of animals & humans caused by bacterium Francisella tularensis. Rabbits, hares, & rodents are especially susceptible & often die in large numbers during outbreaks. Humans can become infected through several routes, including:
- Tick & deer fly bites
- Skin contact with infected animals
- Ingestion of contaminated water
- Inhalation of contaminated aerosols or agricultural dusts
- Lab exposure
Symptoms vary depending on route of infection. Although tularemia can be life-threatening, most infections can be treated successfully with antibiotics.
Steps to prevent tularemia include:
- Use of insect repellent
- Wearing gloves when handling sick or dead animals
- Avoiding mowing over dead animals
- 364D rickettsiosis (Rickettsia phillipi, proposed) is transmitted to humans by Pacific Coast tick (Dermacentor occidentalis ticks). This is a new disease that has been found in California.
- http://www.cdc.gov/otherspottedfever
- In addition to Rickettsia rickettsii, agent of Rocky Mountain spotted fever (RMSF), several other tick-borne species of Rickettsia, broadly grouped under heading "Spotted Fever group Rickettsia (SFGR)" have been shown to cause human infections. Tick-borne SFGR are transmitted to humans by bite of an infected tick, & may cause similar signs & symptoms to those observed for RMSF. These pathogens include several species of Rickettsia found in United States, including R. parkeri & Rickettsia species 364D (Table1). In addition, numerous tick-borne SFGR pathogenic to humans have been described internationally, including but not limited to R. conorii & R. africae (Table 2). Travelers may be at risk for exposure to these pathogens when engaging in behaviors that place them at risk for tick exposure, & physicians should maintain awareness of these diseases when a patient presents with a febrile illness within 2 weeks of returning home. Rickettsial infections with R. africae have been reported as a common cause of fever in travelers returning from South Africa.
- 2016 HHS joint webinar: Trends in Tickborne Diseases - Video
by the Centers for Disease Control & Prevention (CDC)
Published on Aug 16, 2016HHS Working Group on Lyme & Other Tickborne Diseases webinar: Trends in Tickborne Diseases in United States Experts in field of tickborne diseases - https://youtu.be/p6ZlEcaJDrw
- 2013 HHS joint webinar on Novel & Emerging Tickborne Diseases: Agents, Clinical Features, & Surveillance - VideoThis webinar features: Dr. Aaron DeVries from Minnesota Department of Health speaking about Powassan virus disease; Dr. Roger Nasci of CDC speaking about heartland virus; Dr. Peter Krause from Yale School of Medicine describing Borrelia miyamotoi, Dr. Jennifer McQuiston of CDC discussing Ehrlichia muris-like organism; Dr. Barbara Herwaldt of CDC providing an update on Babesia microti, & Anna Perea of CDC describing CDC's tickborne disease prevention resources.
by the Centers for Disease Control & Prevention (CDC)
Published on Jul 11, 2014https://youtu.be/-pWpKdl-tsA
6/11/16
tick articles - North Carolina, Wisconsin

tick articles
https://theconversation.com/us/topics/ticks
ticks in north carolina
http://www.northcarolinahealthnews.org/tag/ticks
ticks in wisconsin
http://host.madison.com/wsj/news/local/health-med-fit/ticks-that-can-carry-lyme-disease-becoming-abundant-in-madison/article_18c2d65f-0cb0-5a6f-9983-6a788e4020f4.html
Tick that can cause meat allergies showing up in Michigan
Tick that can cause meat allergies showing up in Michigan
http://www.mlive.com/news/grand-rapids/index.ssf/2016/05/tick_that_can_cause_meat_aller.html

Tick affliction -- Warm winter, wet spring ideal for ticks
Tick affliction -- Warm winter, wet spring ideal for ticks
http://www.mccookgazette.com/story/2312607.html
What to Do if You Find A Tick on Yourself or on Your Child
What to Do if You Find A Tick on Yourself or on Your Child
http://www.huffingtonpost.com/news/ticks
/
http://www.huffingtonpost.com/news/ticks
/
Subscribe to:
Posts (Atom)


